Case of a 65 year old male with cardiovascular and neurology complaints
An interesting case of a 65 year old male with cardiovascular and neurology complaints
Submitted by- Simran Dash
MBBS-IV | Roll number- 153
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and diagnosis and come up with a treatment plan.
The entire real patient clinical problem is presented in the following link-
My analysis for this patient is as follows-
Age- 65 years
Sex- Male
Occupation- Shepherd (quit working a few years back)
Chief complaints:
- Palpitations
- Dyspnea
- Weakness in lower limbs since 15 days (Paraparesis)
Complaint in detail-
- Palpitations:
- Onset- Sudden at the age of 30 years
- Duration- 25 years
- Progression- Gradually Progressive (from once in 2-3 months to once a week after 5 years of first onset)
- Character- Pounding
- Aggravating factors- exertion
- Relieving Factors- Rest
- Associated complaints- Heaviness in chest
This pattern of Palpitations is highly suggestive of a cardiac etiology. And the pounding character makes it more likely to be a Volume overload case. Most common causes of Volume overload in this case with a chronic etiology are-
- Heart Failure
- Cirrhosis
- Renal Failure
- Anemia
- Aortic regurgitation
- Mitral regurgitation
2. Dyspnea:
- Onset- insidious
- Duration- 20 years
- Progression- Gradually progressive from NYHA 2 To NYHA 3 over several years into his early 50s. This made him quit work. Also made him emotionally unstable.
- Associated complaints- 2 episodes of Paroxysmal Nocturnal Dyspnea. He had his first episode 5 years ago and it got relieved on walking for some distance. This was associated with profuse sweating.
This could be because of sympathetic overdrive causing sweating as in
- Stress
- Anxiety (as he stopped working he could have developed anxiety.)
3. Paraparesis:
- Onset- insidious
- Duration- 15 days
- Progression- Gradually progressive. Increased in the last 5 days to an extent that he was unable to get up from bed and from sitting position.
- Associated complaints-
- Difficulty in squatting (weakness of proximal muscles)
- Severe aching pain in lower limbs (more in left lower limbs than right side)
- Fatigue which is gradually increasing
- Unable to lift his hands above his head without difficulty.
- Unable to comb his hair without difficulty.
- Could not support himself with hands on bed when sitting.
- Constipation since 4 days
- Not associated with -
- Tingling
- Parasthesia
- Muscle atrophy
- No cramps or exercise induced pains
- No difficulty in mixing food or buttoning unbuttoning of shirt.
- No slippage of footwear.
- No diurnal variation.
- Myasthenia Gravis
- Radiculopathy (because isolated muscles are not involved.)
Past history: Had an injury to Right hip because of excess alcohol consumption. This led to taking painkiller (most probably an NSAID) almost everyday orally or injections for 5 years. He also developed pain in his knees and low back.
Personal History: Consumption of alcohol was increased significantly from once a month to daily. He consumes local whiskey- 90 mL daily.
So after the history I am of the opinion that this is a myopathy. Possible explanations which could fit in this case could be-
- Polymyositis
- Sporadic inclusion body myositis
- Necrotizing autoimmune myopathy
On examination, the positive findings are-
General Examination: He is thin built and moderately nourished.
Vitals:
- Pulse Rate- 76 bpm, High volume pulse, collapsing water hammer pulse
- BP- 130/60 (wide pulse pressure of 70 mm Hg )
The possible causes for this could be-
- Valvular regurgitation (Aortic regurgitation more likely)
- Severe iron deficiency anemia
- Aortic stiffening
- Hyperthyroidism
CVS-
- S1, S2 heard with an early diastolic murmur in Aortic area.
- JVP- Pulsus bisfiriens
- Duroziez sign was positive.
These signs indicate Aortic Regurgitation.
CNS-
- Tone was decreased in both the lower limbs.
- Power was 3/5 in Right side and 0/5 in left side (lower limbs)
- All the superficial and deep tendon reflexes are normal
- Ankle jerk was absent.
- Plantar response was extensor (i.e. positive Babinski's sign)
- Beevor's sign was positive.
- On sensory examination,
- Vibration and proprioception were lost in lower limbs.
- Tenderness in dorsal and lumbar region.
- Pain and temperature sensation were preserved.
These findings indicate that the possible anatomical location could be in the posterior coulmns of spinal cord or medial lemniscus of medulla oblongata.
"Disease involving the medial portions of the medulla affects the medial lemniscus, causing contralateral loss of position sense and vibration sense without loss of pain or temperature sensation. As the medial lemniscus of the left and right sides lie immediately adjacent at lower brainstem levels, impairment of position sense and vibration sense often occurs bilaterally."
The possible pathologies responsible for this could be-
- Degenerative lesions
- Nutritional deficiency
- Vascular
- Neoplastic
Etiologies responsible could be-
- Tabes dorsalis - a manifestation of tertiary syphilis
- Vitamin B12 Deficiency causing Subacute combined degeneration of spinal cord.
- Infarction in the posterior spinal artery causing posterior cord syndrome.
- Lymphomas
- Copper deficiency could also cause this.
- Sarcoidosis
Investigations done on this patient are-
- CBP- Hb level: 8.8 gm/dl
There is anemia.
- CUE-
- Albumin: Positive
- Pus Cells: 5-6/hpf
- Epithelial cells: 4-5/hpf
There is albuminuria.
- RFT-
- Urea:49 mg/dl
- Uric acid: 4.4 mg/dl
- Creatinine: 1.0 mg/dl
- Calcium: 9.7 mg/dl
- Phosphorus: 3.7 mg/dl
- Sodium: 141 mEq/L
- Potassium: 3.7 mEq/L
- Chloride: 101 mEq/L
Normal Renal function tests.
- LFT-
- Total bilirubin-1.05 mg/dl
- Direct bilirubin- 0.37 mg/dl
- AST- 19 IU/L
- ALT- 10 IU/L
- Alkaline Phosphatase- 356 IU/L
- Total proteins- 6 gm/dl
- Albumin- 3.7 gm/dl
- A/G Ratio- 1.71
Elevated Alkaline phosphatase levels.
- Serum Creatinine Kinase levels- 36 IU/L (Normal)
- 2D ECHO-
- EF is 55 % (preserved)
- Dilated IVC OF 1.9CM,
- Dilated RA
- RSVP-38MMHG
- Mild TR with mild PAH, Trivial AR
- Good LV systolic function,
- No RWMA Diastolic Dysfunction
- Rapid Plasma Reagin (RPR) was done to rule out the possibility of Tabo paresis.
- Ultra sound-
There was grade 2 prostatomegaly so a urology consultation was taken and got a Digital Rectal Examination(DRE) was done.
DRE revealed a flat and non nodular prostate.
- ECG-
Normal rate of 69 bpm and regular rhythm
There is hilar congestion, cephalization, Kerley B lines.
These findings are suggestive of pulmonary edema which could be due to Aortic Regurgitation.
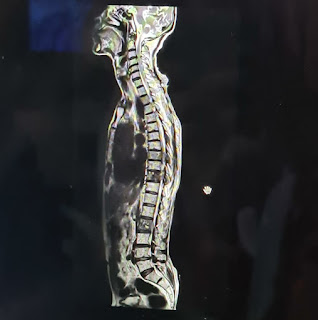
Vertebral lesions at D8,D10,L2 which are causing the cord compression.
After all the investigations, I came to the conclusion that he could have-
- Myeloneuropathy secondary to spinal cord compression which is caused by the metastatic lesions at D8,D10,L2 vertebrae.
- Aortic regurgitation with mild Pulmonary artery hypertension.
- Grade 2 prostatomegaly i.e. BPH
The additional investigations needed for him are-
- Prostate specific antigen test to rule out prostate cancer.
- Serum Vitamin B12 levels to rule out B12 deficiency
- Serum methylmalonic acid levels to rule out B12 deficiency
- Peripheral smear
- Bone marrow examination to rule out lymphomas.
- FNAC to rule out other malignancies.
- Electromyography and Nerve conduction study should also be done to rule out Myopathy.
- Urinalysis for blood and bacteria to confirm BPH.
- Copper levels should also be examined in serum.
- Biopsy of lung tissue to confirm sarcoidosis.
Treatment received by him-
- INJ THIAMINE 1 AMPULE IN 100ML NS/IV/BD
- INJ OPTINEURON 1 AMPULE IN 100ML NS/IV OD
- TAB CIPROFLOXACIN 500 MG PO/BD. 3 DAYS
- SYRUP LACTULOSE 20 ML PO/BD
Additional treatment required are:
- Pharmacological-
- Alpha 1 blockers like Prazosin, tamsulosin for BPH.
- For sarcoidosis-
- Immunosuppressants like Azathioprine
- Corticosteroids
2. Non Pharmacological-
- Maintaining a healthy lifestyle.
- Avoiding alcohol.
- Physical therapy is recommended to prevent muscle atrophy.
- Eating a healthy diet
- Managing stress.
- Mobilisation
- Clinical methods of medicine by Arup kumar Kundu
- Hutchison’s clinical methods
- Davidson's principles and practice of medicine
- Harrison's Principles of internal medicine




Comments
Post a Comment